What are the Causes of Snoring?
When you’re awake and breathing normally, the muscles surrounding the soft tissues at the back of your throat hold open the airways. This allows air to flow easily in and out from your nose or mouth to your lungs. Unless you’ve been exerting yourself, or have some respiratory problem, the act of breathing is usually very quiet.
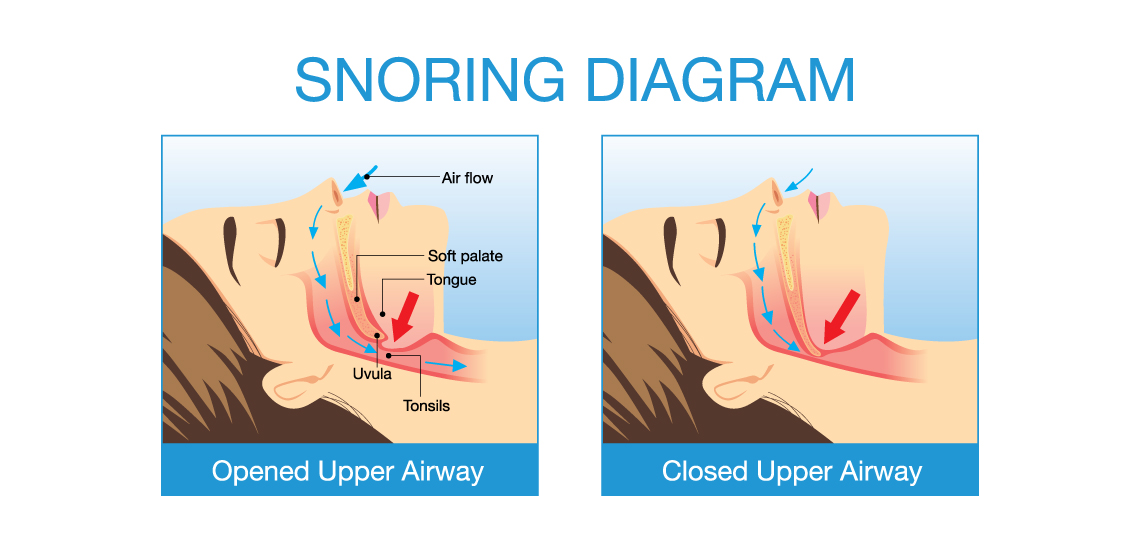
It’s estimated that 45% of men and 30% of women regularly snore. While in some people snoring is due to a nasal problem, for the vast majority it occurs when the soft tissues of the throat collapse during sleep. As a result, when the body attempts to move air in and out of this area, the tissues vibrate against each other, producing the snoring sound. Other factors that can contribute to a narrowing of the airway include:
- large tonsils
- a long soft palate
- a large tongue
- a larger or longer than average uvula (that’s the dangly tissue hanging down from the back of the throat), and excess fat deposits in the throat.
In general, the narrower your airway, the louder or more prolonged your snoring.
When is snoring a sign of obstructive sleep apnoea?
During deep sleep, and especially if you sleep on your back, your jaw can become relaxed and drop down. If your airway is already narrowed, this will constrict it even further, making it harder to breathe in and out. Once the brain senses a reduction of the oxygen levels in your blood, it kick-starts your breathing by interrupting your sleep cycle and bringing you back to a lighter sleep (or even waking you up).
Obstructive sleep apnoea is the name given to the condition where the muscles relax so much that the airway is completely restricted and breathing stops for 10 seconds or more. Each episode can last up to two minutes and a person is diagnosed as having obstructive sleep apnoea if they experience more than five episodes an hour.
Sometimes the end of an episode results in the person waking up, but often they’ll be unaware of the episodes, and simply feel that they haven’t rested properly. If you’re listening to someone snore, obstructive sleep apnoea is often indicated by irregular pauses in their snoring – when it may seem they have stopped breathing – which are then followed by a gasping or choking sound as the airways reopen and the body rapidly inhales.
There are two other types of apnoea. ‘Central apnoea’ is not usually associated with snoring, and occurs due to the part of the brain that controls breathing, failing to function properly, causing breathing to stop momentarily. ‘Mixed apnoea’ is a combination of central and obstructive apnoea and usually involves snoring.
Treatment for Snoring and Obstructive Sleep Apnoea
There are three main ways of treating snoring and obstructive sleep apnoea:
- Oral appliance therapy – where a custom made dental device is fitted in your mouth to prevent the airways from collapsing. The type of device used will depend on your specific dental or medical needs.
- Continuous positive airway pressure (CPAP) – this treatment method requires wearing a mask that fits over your mouth and nose, or just over your nose, while sleeping. It is the most common treatment for moderate to severe obstructive sleep apnoea in adults.
- Surgery – for some people, one of several surgical procedures may provide the best treatment for sleep apnoea. These procedures may include widening the breathing passages, removing tonsils, reducing the tongue size – and more.
Here’s a little more detail on each specific treatment method.
Snoring Therapy by Oral Appliance
If you have mild-to-moderate obstructive sleep apnoea, an oral dental device is a safe, painless and effective treatment that provides a mechanical method for holding the airway open while you’re sleeping.
When making and fitting an oral appliance, your Holistic Dental practitioner will first draw on their experience in treating temporomandibular joint disorders (TMJ), and take into consideration the position and structure of your jaw, and the impact this has on your breathing. They will also take X-rays and make an impression of your teeth to ensure the device fits perfectly.
There are several different types of oral dental appliances available, however the main two are:
- A mandibular advancement device (MAD) – This is the commonly used oral treatment for obstructive sleep apnoea and looks much the same as a sports mouthguard. The device works by forcing the lower jaw forward and slightly downward to ensure the airway is kept open.
- A tongue retraining device (TRD) – This oral device is used when the airways is being blocked by the tongue falling backward while you’re sleeping. The device uses a splint to hold the tongue in place, which in turn helps keep the airway clear and open.
Oral appliances are small and light (so you can easily take them with you when travelling), reasonably inexpensive and easy to wear. With most, it’s possible to speak or even drink while wearing them, and if they are cleaned and stored correctly, are long lasting.
Some of the side-effects you may experience include:
- Dry mouth and/or lips
- Excessive salivation
- Night-time pain
- Tooth discomfort.
Once your oral appliance has been fitted, you should have it regularly checked by your Holistic Dental practitioner to make certain it is working correctly and fitting properly. It’s also important to let your Holistic practitioner know if you’re experiencing any discomfort, irritation or changes to your bite. This is extremely important, because long term use may lead to permanent changes to your teeth or jaw if the device is not adjusted, or replaced, when required. (In some cases these changes are part of the desired result of the treatment; however in all cases ongoing monitoring and maintenance are vital.)
Finally, oral appliance therapy may not be suitable if you have a pre-existing disorder of the temporomandibular joint (TMJ or jaw joint); severe untreated gum disease or dental decay; or full dentures. Your Holistic Dental practitioner can advise you about the best treatment options available to you in these circumstances


